Advanced Surgical Treatments
Dr. Womack's 2-year Minimally Invasive Gynecologic Surgery (MIGS) fellowship gives her advanced experience surgically managing complex gynecologic diseases. She is able to offer major surgeries through small incisions which allow you to go home the same day. Minimally invasive surgeries have lower blood loss, infection rates, and hospital stays compared to open surgeries. Her minimally invasive techniques also focus heavily on adhesion reduction and fertility restoration for those couples struggling with infertility.
Endometriosis Excision
Endometriosis is defined as tissue similar to endometrial glands and stroma (tissue normally on the inner wall of the uterus) that grow outside of the uterus. Common places endometriosis can grow are the pelvic walls, ovaries, behind the cervix, and rectum.
-
Learn More
Endometriosis can cause a constellation of symptoms including (but not limited to):
- Painful periods
- Painful sex
- Painful bowel movements
- Fatigue
- Bloody stools or urine
- Gastrointestinal issues
- Bloating
- Infertility
- Recurrent miscarriages
Did the you know that, even with all these symptoms, the average time to diagnosis of endometriosis is 8 to 10 years from time of presentation to care? Women deserve better!
The only way to officially diagnose endometriosis is through a laparoscopic surgery where we take a biopsy of tissue to confirm endometriosis. At the same time, I can also treat your endometriosis. The goal of surgery is optimal excision, which means that we want to remove all visible disease, not just ablate or fulgurate it.
As an endometriosis excision expert, I am trained to find not only the obvious endometriosis lesions, but also the ATYPICAL lesions that are often missed. This recognition is crucial to achieving optimal excisions and lasting results.
BONUS: My goal is to also prevent adhesion formation, optimize fertility, and leave your pelvis in better shape than when I found it. See the section of Adhesion Prevention for more details.
Why come to me for endometriosis surgery?
I am trained to find both typical and atypical endometriosis implants.
I excise endometriosis implants rather than fulgurate them.
I use fine and delicate surgical techniques to prevent tissue damage and adhesion formation.
I utilize several strategies for adhesion prevention in order to optimize pelvic health.
I understand the need for rehabilitation and care after endometriosis surgery.
Myomectomy Fibroid Removal
Fibroids, or leiomyomas, are benign tumors of the muscle of the uterus that are stimulated by estrogen. Fibroids are fairly common, but not all of them cause issues that need to be addressed. There is a wide variety of fibroid types characterized by size and location.
-
Learn More
We can definitely see fibroids on a pelvic ultrasound. If we plan on a myomectomy, or removing the fibroids, then we get a pelvic MRI to map the fibroid locations for removal.
Depending on the type of fibroid that you have, you may have any of the following symptoms:
- Heavy periods
- Pelvic pressure
- Urinary frequency
- Constipation
- Painful sex
- Pelvic pain
- Recurrent miscarriages
- Infertility
How do we treat fibroids? There are so many ways that we can address fibroids, and the best choice depends on the type of fibroid and fertility goals. Treatments can include:
- Laparoscopic myomectomy
- Hysteroscopic myomectomy
- Hysterectomy
- Uterine artery embolization
- Radiofrequency ablation
Cesarean Scar-Defect Repair
Did you know that almost one third of babies in the United States are born by c-section? While c-sections can be wonderful aids to a healthy-mom-healthy-baby delivery, they can pose some issues postpartum if someone develops a cesarean scar defect.
-
Learn More
A c-section scar defect is also called an "isthmocele" or a "uterine niche". This defect presents as a pocket in the inner lower segment of the uterus where the incision on the uterus was during c-section. Of course, not all women will have issues from said defect, but a niche can cause inflammation, bothersome bleeding/spotting, and/or fertility issues.
How can we diagnose a cesarean scar defect?
In general, a defect is diagnosed by ultrasound. I evaluate the inner cavity of the uterus with a saline-infused sonogram (SIS) which fills the uterus with fluid while we do an ultrasound in order to see the defect. I can then measure its dimensions.
At times, these defects will require repair which can be done hysteroscopically or laparoscopically. The approach depends on the size and depth of the defect as well as future fertility goals.
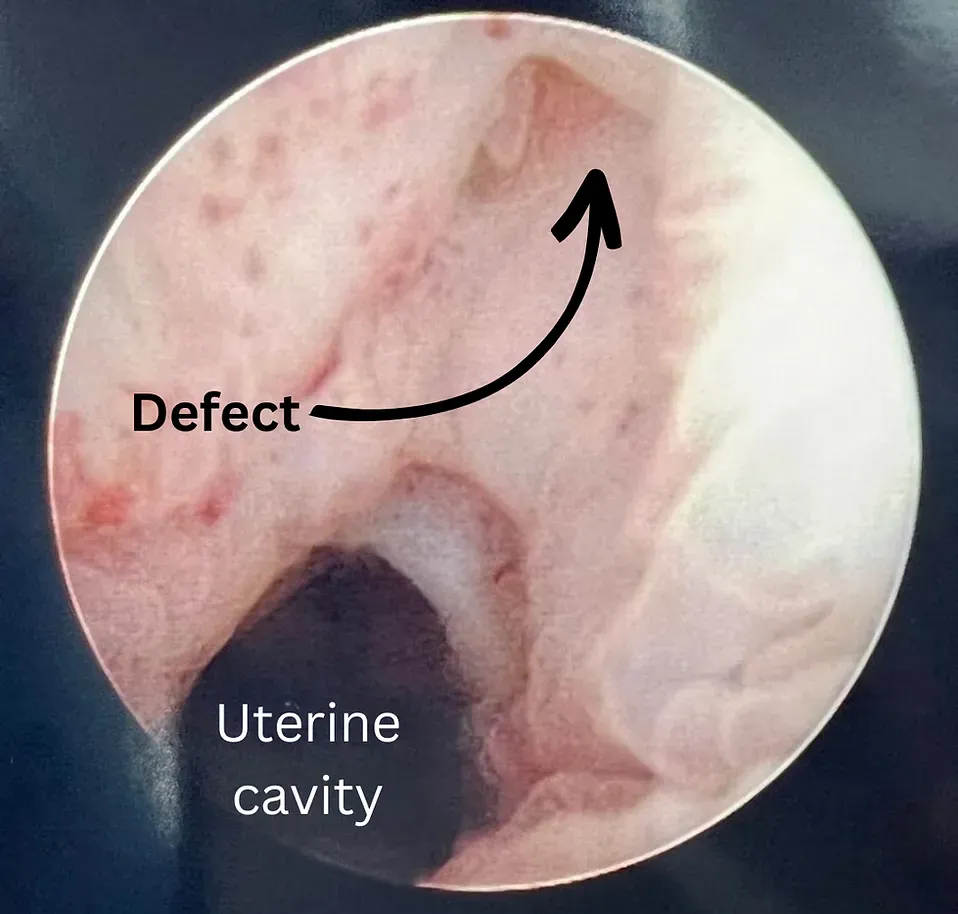
Here you can see the defect hysteroscopically (camera inside the uterus) which helps me to pinpoint it laparoscopically (inside the abdomen) and fully resect and repair it!
Creighton Model charting can show signs of a uterine niche which is another great reason to chart and track your cycles!!
Slide title
Write your caption hereButton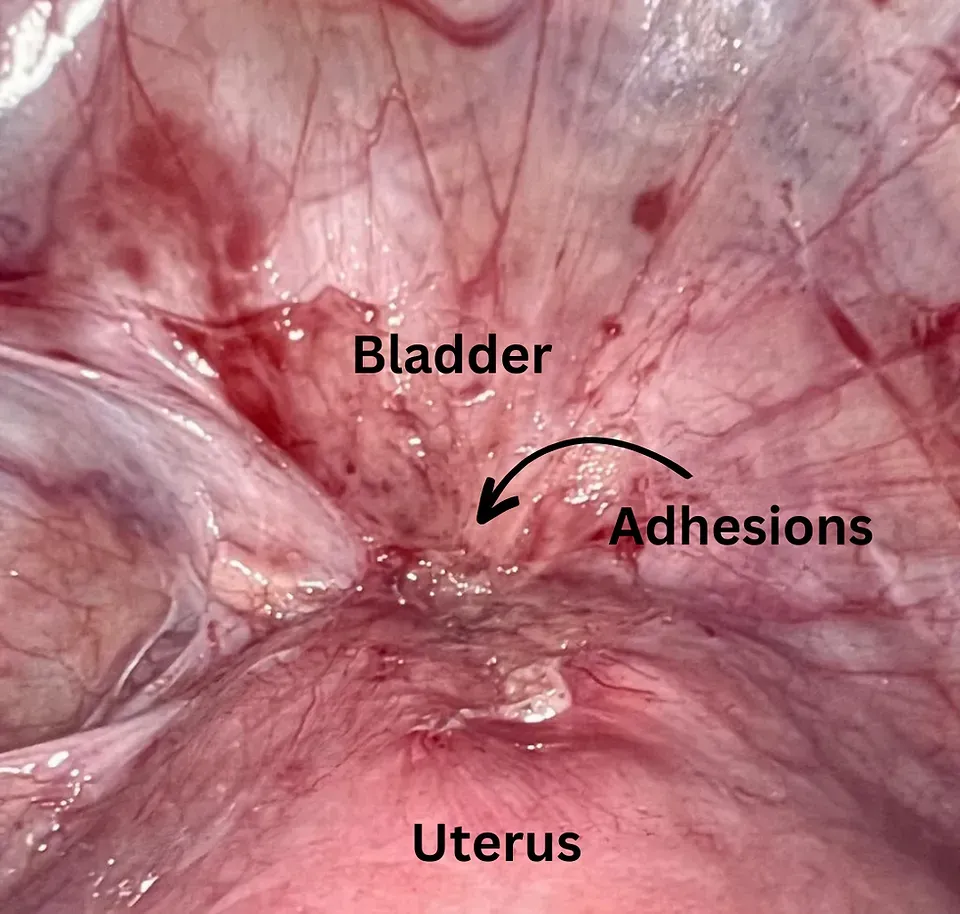
Slide title
Write your caption hereButton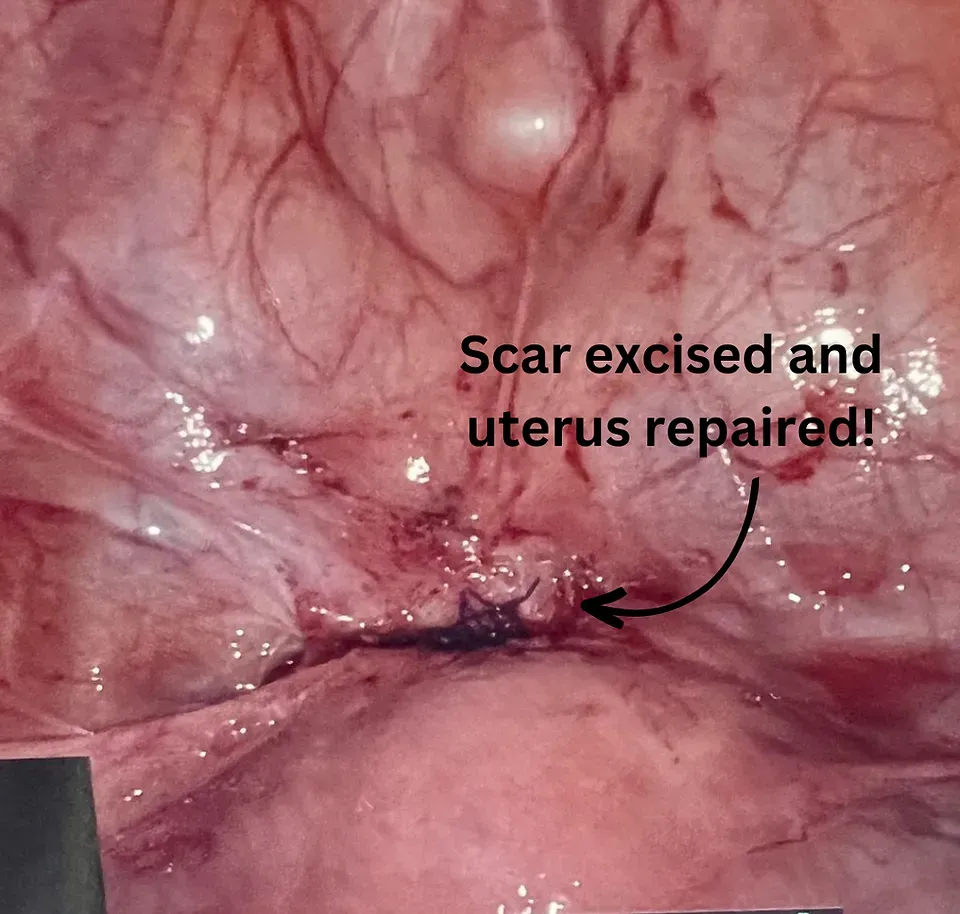
Slide title
Write your caption hereButton
More Surgical Treatments
- Robotic surgery
- Advanced hysteroscopy
- Myomectomy (fibroid removal)
- Excision of endometriosis
- Robotic, laparoscopic, and vaginal hysterectomy
- Ovarian cyst removal
- Ovarian wedge resection
- Tubal reversal
- Tubal recanalization
- Cesarean scar defect (isthmocele) removal
- Robotic transabdominal cerclage
- Vaginal cerclage
- Labioplasty
- Vaginal surgery
- Pelvic floor trigger point injections
- Pelvic floor Botox injections
- Endometrial ablation
- Uterine / cervical polypectomy
- Lysis of uterine adhesions
- Lysis of pelvic adhesions
Call Us
Fax
214-305-7799
Our Address
8160 Walnut Hill Ln. Suite 320
Dallas, TX 75231
info@pearlhealthdallas.com
Call Us
Fax
214-305-7799
Our Address
8160 Walnut Hill Ln,
Dallas, TX 75231 USA
Suite 320


